Every person is different. We can try to generalize various things and it is important to have general treatment protocols for various sicknesses, diseases, and other issues, for example, for multiple sclerosis. But because every single body is unique in its way, just because something worked for 100 people doesn’t mean that it would work for you due to additional factors like background, concomitant diagnoses, cultural context, and a multitude of other things.
As a result, to improve the treatment’s efficiency, the doctors have to personalize their approach to medicine. Not just a generic knowledge of “this cures this, here you go” but going deeper into the patient’s health history to ensure that medicines won’t, for example, counteract one another.
Medicine Personalization Statistics
Market Growth:
- Global Personalized Medicine Market: As of 2021, the global personalized medicine market was estimated to be worth around USD 60 billion, with forecasts suggesting a growth to USD 140 billion by 2022 [Source: Statista].
- AI in Healthcare: The global Artificial Intelligence in the healthcare market was over USD 11 billion in 2021 and is projected to reach around USD 188 billion by 2030.
Impact on Treatment:
- Number of Personalized Medicines: In the United States, the number of personalized medicines on the market more than doubled between 2016 and 2020, with personalized medicines accounting for 25% of new drugs approved by the FDA in 2019 [Source: AJMC]
- Increased Efficiency and Accuracy: AI can analyze vast amounts of medical data to identify patterns and trends that help doctors make more accurate diagnoses and personalized treatment plans. Studies suggest AI can achieve better accuracy in disease detection compared to traditional methods [Source: Various sources depending on specific disease, for example, a 2023 study published in Nature Medicine found AI outperformed doctors in detecting diabetic retinopathy].
Shift in Doctors’ Approach:
- Focus on Precision: Personalized medicine with the help of AI allows doctors to move away from a one-size-fits-all approach to treatment and focus on tailoring treatments to individual patients based on their unique genetic makeup, lifestyle factors, and medical history.
- Improved Patient Outcomes: Personalized medicine can improve patient outcomes by focusing on targeted treatments with a higher chance of success and fewer side effects.
Why is personalization so important?
Tailored Treatment Plans
Every patient is unique, with individual genetic makeup, medical history, lifestyle factors, and preferences. Personalization allows healthcare providers to develop treatment plans specifically tailored to each patient’s needs, increasing the likelihood of successful outcomes. Yes, generic protocols remain the same, but unfortunately, most of the time, there is not just one sickness that is attacking the body.
Optimized Medication and Dosage
Personalized medicine considers factors such as genetic variations and medication responses to determine the most effective drugs and dosages for individual patients. This approach minimizes the risk of adverse reactions and improves medication adherence. For example, this is true for managing and tracking blood pressure, thyroid hormone levels (if the patient has to take pills after having the thyroid itself removed), or antidepressants.
Precision Diagnosis and Early Detection
Treating something at its very beginning (or even before it began based on the information available from the tests) is always easier than when the disease or condition has progressed. Personalized diagnostics leverage advanced technologies, such as genetic testing and molecular profiling, to identify diseases at earlier stages and with greater accuracy. Early detection enables timely interventions, potentially preventing disease progression and improving prognosis.
Improved Patient Engagement and Adherence
People like to be treated like people, not just “work subjects.” When patients feel that their healthcare providers understand their unique circumstances and needs, they are more likely to actively participate in their treatment plans and adhere to medical recommendations. Personalization fosters stronger patient-provider relationships and enhances engagement in healthcare decision-making.
Reduced Healthcare Costs
By targeting treatments and interventions based on individual characteristics, personalized medicine can help reduce unnecessary procedures, minimize trial-and-error approaches to medication management, and prevent hospital readmissions. This, in turn, leads to cost savings for healthcare systems and payers.
Empowerment and Patient-Centered Care
Patient experience (as well as doctor/nurse experience) matters. Personalization shifts the focus of healthcare from a one-size-fits-all approach to a patient-centered model that prioritizes individual preferences, values, and goals. Empowering patients to actively participate in their healthcare decisions promotes autonomy, dignity, and overall well-being. For example, this works well in nursing homes, when patients can feel like they still have some sort of control over their lives and not just trying to exist.
How to implement a personalized approach in healthcare practices?
The first and primary advice is to remember we are all human.
Basic, yes, but at the same time, very poignant. In our day and age when everything becomes digital, it is important to retain that humanity in everything we do. This concerns doctors, nurses, as well as patients and their family members. Mutual respect and being available to hear what the other person is saying helps to personalize the approach more than anything else.
Patient’s side
Before we go to the part that doctors and medical staff are more involved in, here are a few things that patients and their family members can do to help medical staff find the best-fitting correct treatment:
Medical staff’s side
Doctors, nurses, and medical staff also are encouraged to use a people-oriented personalized approach. This can be done in many ways:
How can artificial intelligence help?
The advancements in artificial intelligence (AI) are reshaping the landscape of personalized medicine. Medical staff is pretty much always short on time and patients are many. Therefore it is often hard to take into account all the factors and information people are sharing, even if the doctor is actively listening and writing down information.
Some of the connections are not as clear from the very beginning and this is where software, machine learning, and AI technologies can help to analyze and process this data to provide valuable insights.
There are four major areas where AI and machine learning can be helpful:
Precision Diagnosis
IBM Watson for Oncology is an AI-powered diagnostic tool designed to assist oncologists in providing personalized cancer treatment recommendations.
By analyzing a patient’s medical records, including pathology reports, medical imaging, and genetic data, Watson for Oncology can identify treatment options based on the latest medical literature and clinical guidelines.
This helps oncologists make more informed decisions about treatment plans tailored to each patient’s specific cancer type, stage, and genetic profile.
IDx-DR is another AI-based diagnostic system designed to detect diabetic retinopathy, a leading cause of blindness, through the analysis of retinal images. The system uses deep learning algorithms to evaluate images of the retina captured with a fundus camera and identify signs of diabetic retinopathy, such as microaneurysms and hemorrhages. IDx-DR can provide accurate diagnostic results within minutes, enabling timely intervention and referral to ophthalmologists for further evaluation and treatment. By automating the screening process, IDx-DR helps healthcare providers efficiently identify individuals at risk of vision loss due to diabetic retinopathy, leading to improved patient outcomes and reduced healthcare costs.
Predictive Analytics
Heart Disease Risk Prediction Models
Various predictive models have been developed to assess an individual’s risk of developing heart disease based on factors such as age, gender, blood pressure, cholesterol levels, smoking status, and family history of cardiovascular disease.
These models, including the Framingham Risk Score and the Reynolds Risk Score, use statistical algorithms to calculate a person’s probability of experiencing a heart attack or stroke within a specified time frame. By identifying individuals at higher risk, healthcare professionals can implement preventive measures such as lifestyle modifications, medication therapy, and regular cardiovascular screenings to reduce the likelihood of adverse cardiovascular events.
Diabetes Risk Assessment Tools
Predictive models have been developed to evaluate an individual’s risk of developing type 2 diabetes mellitus based on demographic characteristics, lifestyle factors, medical history, and biomarkers such as fasting glucose levels and body mass index (BMI).
For example, the Finnish Diabetes Risk Score (FINDRISC) and the American Diabetes Association (ADA) Risk Test utilize algorithms to estimate an individual’s probability of developing diabetes over a specified period. Healthcare providers can use these risk assessment tools to identify individuals at increased risk of diabetes and implement targeted interventions such as dietary counseling, weight management programs, and glucose monitoring to prevent or delay the onset of the disease.
Sepsis Prediction Algorithms
Sepsis is a life-threatening condition characterized by a dysregulated immune response to infection, and early detection is crucial for timely intervention and improved outcomes.
Predictive models, such as the Sequential Organ Failure Assessment (SOFA) score and the Modified Early Warning Score (MEWS), use clinical variables including vital signs, laboratory values, and patient demographics to assess the likelihood of sepsis development or progression.
By continuously monitoring patients for signs of clinical deterioration and utilizing predictive algorithms to identify individuals at high risk of sepsis, healthcare professionals can initiate early interventions such as antibiotic therapy, fluid resuscitation, and intensive care unit (ICU) admission to prevent sepsis-related complications and reduce mortality rates.
Treatment Optimization
AI plays a vital role in optimizing treatment plans by considering factors such as genetic predispositions, medication responses, and lifestyle factors, ultimately leading to more effective and personalized care. For example,
Pharmacogenomics and Drug Response Prediction
AI-powered pharmacogenomic platforms analyze an individual’s genetic makeup to predict how they will respond to specific medications. For instance, platforms like Myriad Genetics’ GeneSight use machine learning algorithms to interpret genetic variations related to drug metabolism and neurotransmitter pathways.
By considering genetic predispositions, these platforms help healthcare providers identify medications that are likely to be most effective and well-tolerated for each patient, thereby optimizing treatment outcomes and minimizing adverse drug reactions.
Personalized Cancer Treatment
AI-based oncology platforms integrate genetic and molecular data with clinical information to guide personalized cancer treatment decisions. For example, platforms like Tempus and Foundation Medicine use machine learning algorithms to analyze tumor genomic profiles and identify potential treatment options, including targeted therapies and immunotherapies.
By considering genetic alterations and tumor characteristics, these platforms enable oncologists to tailor treatment plans to each patient’s unique cancer biology, improving treatment response rates and survival outcomes.
Digital Health Coaching and Behavior Modification
AI-driven digital health coaching platforms leverage patient-generated data and behavioral insights to deliver personalized interventions for chronic disease management. For instance, platforms like Livongo and Omada Health use machine learning algorithms to analyze patient data, including blood glucose levels, physical activity patterns, and dietary habits, to provide tailored recommendations and support for individuals with diabetes, hypertension, and other chronic conditions.
By considering lifestyle factors and individual preferences, these platforms empower patients to make sustainable behavior changes and achieve better health outcomes, ultimately leading to more effective and personalized care.
Remote Monitoring and Telemedicine
One example highlighting the use of AI-driven remote monitoring devices and telemedicine platforms is the “BioSticker” by VitalConnect.
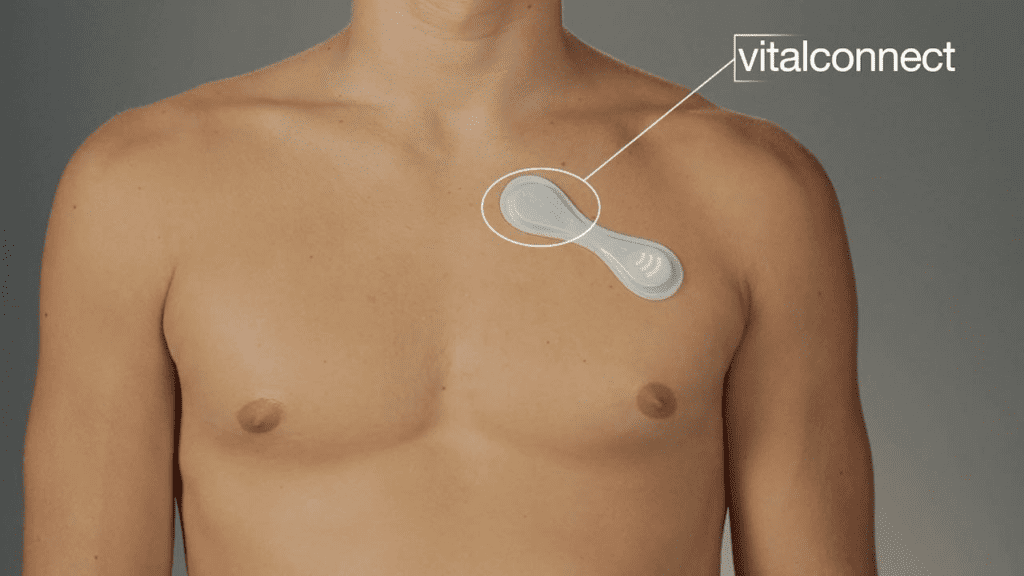
The BioSticker is a wearable, adhesive biosensor that continuously monitors a range of physiological parameters, including heart rate, respiratory rate, skin temperature, and activity levels. The device utilizes advanced AI algorithms to analyze the collected data in real time and detect anomalies or trends that may indicate changes in the patient’s health status.
Healthcare providers can remotely access the patient’s data through a secure cloud-based platform, allowing for continuous monitoring and early detection of potential health issues. By leveraging AI-driven analytics, clinicians can receive alerts for abnormal vital signs or deviations from baseline values, enabling timely intervention and proactive management of patients’ health conditions.
The BioSticker’s capabilities facilitate remote patient monitoring, particularly for individuals with chronic conditions, post-operative care needs, or those at risk of health complications. By reducing the need for frequent in-person visits and enabling proactive intervention, BioSticker, and similar AI-driven remote monitoring devices contribute to improved patient outcomes, enhanced care coordination, and more efficient healthcare delivery.
We wrote more about telemedicine and remote monitoring in our other article on Healthcare Trends in the US.
Ethical and regulatory challenges to consider
The use of AI in healthcare presents various ethical implications and regulatory challenges, including:
Data Privacy
Challenge: AI algorithms require access to vast amounts of sensitive patient data, raising concerns about privacy breaches and unauthorized access.
Solution: Implement robust data encryption and security protocols, ensure compliance with data protection regulations such as GDPR and HIPAA, and obtain explicit patient consent for data collection and usage.
Algorithm Bias
Challenge: AI algorithms may exhibit biases based on the quality and representativeness of the training data, leading to disparities in diagnosis, treatment recommendations, and patient outcomes.
Solution: Conduct thorough data audits to identify and mitigate bias in training datasets, incorporate diverse and representative data sources, and employ fairness-aware algorithms to ensure equitable outcomes for all patient populations.
Patient Consent
Challenge: Patients may not fully understand the implications of AI-driven healthcare interventions or the extent of data sharing involved, leading to concerns about informed consent.
Solution: Enhance patient education and transparency regarding the use of AI in healthcare, provide clear explanations of data collection and usage practices, and enable patients to exercise informed consent through opt-in/opt-out mechanisms and granular data sharing preferences.
Regulatory Oversight
Challenge: Existing regulatory frameworks may struggle to keep pace with the rapid advancements in AI technology, resulting in gaps in oversight and accountability.
Solution: Establish comprehensive regulatory guidelines and standards for the development, validation, and deployment of AI-based healthcare solutions, foster collaboration between regulatory agencies, industry stakeholders, and academic institutions, and promote ongoing monitoring and evaluation of AI systems to ensure compliance with regulatory requirements.
Accountability and Liability
Challenge: Determining accountability and liability in cases of AI-related errors, adverse events, or malpractice poses significant legal and ethical challenges.
Solution: Clarify roles and responsibilities among healthcare providers, technology developers, and regulatory authorities, establish clear protocols for reporting and addressing AI-related incidents, and develop liability frameworks that hold stakeholders accountable for ensuring the safety, reliability, and ethical use of AI technologies in healthcare.
Addressing these challenges requires a multidisciplinary approach involving stakeholders from healthcare, technology, regulatory, and ethics domains. By proactively addressing ethical implications and regulatory challenges, healthcare organizations can harness the transformative potential of AI to improve patient care, enhance clinical outcomes, and uphold ethical standards and patient rights in the digital age.
What does the future hold?
The AI and machine learning technologies will remain for generations to come. Therefore, it’s always better to see the benefits of its implementation early on as well as its potential dangers. Personalized medicine is a truly vital area where data analysis and various visualization tools can become guides for doctors and nurses in treating patients well while spending less time poring over the documents in search of connections.
What is one possible thing to expect to come soon? Virtual Healthcare Assistants. With ChatGPT gaining wild popularity, more and more people are getting interested in consulting an AI tool before going further. While ChatGPT is NOT the best place to search for medical treatments (at least at the moment), I think it would be rather logical to soon have something like this available, considering the amount of data online.
Virtual healthcare assistants driven by AI are poised to play a prominent role in transforming the patient experience and enhancing care delivery. These assistants could take various forms, including chatbots, voice-activated interfaces, and virtual avatars, capable of engaging with patients in natural language conversations, answering questions, providing education, and offering personalized health recommendations based on individual preferences and health data.
Furthermore, virtual assistants could facilitate seamless coordination of care across multiple healthcare providers and settings, streamlining administrative tasks, scheduling appointments, and assisting with medication management. As AI technology continues to advance, virtual healthcare assistants are expected to become increasingly intelligent, empathetic, and context-aware, empowering patients to take an active role in managing their health and well-being while improving access to quality care and reducing healthcare disparities.
In the meantime, we’ve got to remember that while all the artificial intelligence, machine learning, and robotics technologies are wonderful, we are still people. Therefore, personalized medicine is one of the areas where we need to pay more attention, especially since we’ve got the tools.
Wondering about time-to-value?
Request a no-obligation discovery call and receive a preliminary estimate tailored to your KPIs.


